Written by:

Medically Reviewed by:
Last Updated:
February 14th, 2025
Personality Disorder and Addiction
What Is Personality Disorder (PD)?
A personality disorder (PD) is a type of mental health condition that affects how a person thinks, feels and behaves, making it challenging to relate to others and navigate everyday life. People with PD often have long-standing patterns of thinking and behaving that differ significantly from societal expectations, causing distress and difficulties in relationships, work and social settings.
In the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), personality disorders are grouped into three clusters based on similar characteristics:
- Cluster A (Odd or eccentric): Includes Paranoid, Schizoid and Schizotypal Personality Disorders.
- Cluster B (Dramatic or emotional): Includes Borderline, Narcissistic, Histrionic and Antisocial Personality Disorders.
- Cluster C (Anxious or fearful): Includes Avoidant, Dependent and Obsessive-Compulsive Personality Disorders.
Each type has unique features, but all involve persistent difficulties in managing emotions, relationships and self-image.
What are the signs of Personality Disorders?
Recognising the signs of a personality disorder (PD) is crucial, as these conditions often go undiagnosed for many years. The earlier the signs are identified, the sooner treatment can begin, allowing individuals to understand themselves better and improve their quality of life.
Personality disorders affect how people think, feel and behave, often creating challenges in relationships, work and daily life. While the specific symptoms vary depending on the type of PD, here are some common signs to look out for, with examples to provide a clearer picture:
- Unstable relationships: People with PD may find it difficult to maintain long-term relationships due to trust issues, emotional intensity or sudden changes in how they view others. For instance, they might idealise someone one moment and feel deeply betrayed by a small disagreement the next, leading to frequent arguments or breakups.
- Emotional dysregulation: Extreme mood swings, from intense anger or sadness to euphoria, can occur with little warning. A person might feel calm one minute but become overwhelmed by frustration or despair in response to something minor, leaving them and those around them emotionally exhausted.
- Distorted self-image: Someone with PD may struggle with an unclear sense of identity, leading to confusion about their goals, values or purpose. They might frequently change careers, friend groups or hobbies in an effort to “find themselves,” which can leave them feeling lost or unfulfilled.
- Impulsive or risky behaviour: Acting without thinking can manifest in various ways, such as reckless spending, gambling, unsafe sexual practices or substance use. For example, a person might drain their savings on a whim or take unnecessary risks in their personal life, often regretting their actions later.
- Difficulty handling stress or criticism: Even mild stress or perceived criticism can trigger intense reactions, such as withdrawal, anger or feelings of worthlessness. For instance, being overlooked for a promotion might not just feel disappointing but devastating, leading to significant emotional distress.
Is there a link between Personality Disorder and addiction?
Personality Disorder (PD) and addiction often go hand in hand, creating a difficult cycle that can be hard to break. People with PD may turn to substances or addictive behaviours to manage intense emotions, impulsivity or a deep sense of emptiness. While these coping methods might offer temporary relief, they can make PD symptoms worse, leading to even greater emotional struggles and instability in relationships.
Research shows that people dealing with both PD and addiction face unique challenges. For example, alcohol-dependent individuals with personality disorders often experience more severe symptoms, an earlier onset of addiction and higher rates of relapse compared to those without PD. Social difficulties and even suicidal behaviours are sadly more common, adding further complexity to their recovery journey.
Addiction linked to PD isn’t limited to substances—it can also involve behavioural addictions, including:
- Gambling addiction: Nearly half of pathological gamblers meet the criteria for a personality disorder, with Cluster B disorders like PD being particularly common. This can result in cycles of emotional highs and lows linked to wins and losses.
- Internet addiction: Emotional instability and impulsivity associated with PD have been linked to problematic internet use, often as a way to escape overwhelming feelings or stressful life situations.
- Food addiction: People with PD may be more sensitive to rejection, which can trigger emotional dysregulation and lead to disordered eating patterns as a way to find comfort or regain control.
Recognising the link between PD and addiction is essential because both conditions influence one another. Treating them together through compassionate, comprehensive care can make recovery more achievable, helping people build healthier, more balanced lives.
How are Personality Disorder (PD) and addiction treated?
Treating PD and addiction together is a complex but achievable process when approached with care and understanding. People with PD face unique challenges during recovery, such as difficulties forming trust and fears of abandonment, which can make traditional rehab settings more daunting. Addressing these concerns requires a supportive, tailored approach.
If severe PD symptoms, such as those that pose risks to others, are present, it’s crucial to stabilise these first before attempting co-occurring treatment. This ensures the individual is in the right mindset to engage with the recovery process fully.
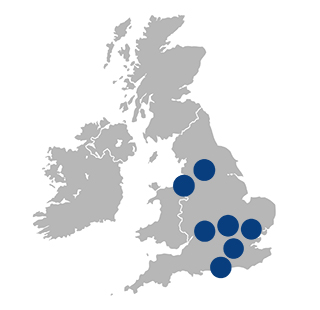
At Liberty House, our treatment programmes combines therapies that address both conditions simultaneously:
- Cognitive-behavioural therapy (CBT): CBT helps identify and reshape negative thought patterns and behaviours. For those with PD and addiction, it can enhance emotional regulation, reduce impulsivity and build strategies to prevent relapse.
- Dialectical behaviour therapy (DBT): Specifically designed for PD, DBT equips individuals with skills to manage intense emotions, improve interpersonal relationships and reduce harmful behaviours, making it a cornerstone of co-occurring treatment.
- Group therapy: A group setting can provide a sense of connection and shared understanding, creating trust and social skills. This is especially beneficial for individuals with PD who may struggle with feelings of isolation.
- One-to-one therapy: Individual sessions offer a safe, confidential space to explore the challenges of managing both PD and addiction, promoting deeper personal growth.
Ongoing aftercare is vital to maintaining recovery, offering continued support to navigate the ups and downs of life while reinforcing the skills learned in therapy. With the right care, individuals can achieve a balanced, fulfilling life.
Take the first step towards a new beginning
If you or someone you love is struggling with Personality Disorder and addiction, don’t wait to seek help. Reach out to Liberty House for expert advice and personalised treatment options. Recovery is possible with the right support, and taking that first step could improve a life. Contact Liberty House today.
Frequently Asked Questions
(Click here to see works cited)
- Kienast T, Stoffers J, Bermpohl F, Lieb K. Personality Disorder and comorbid addiction: epidemiology and treatment. Dtsch Arztebl Int. 2014 Apr 18;111(16):280-6. doi: 10.3238/arztebl.2014.0280. PMID: 24791755; PMCID: PMC4010862.
- Moreira D, Azeredo A, Dias P. Risk Factors for Gambling Disorder: A Systematic Review. J Gambl Stud. 2023 Jun;39(2):483-511. doi: 10.1007/s10899-023-10195-1. Epub 2023 Mar 8. PMID: 36884150; PMCID: PMC9994414.
- Internet Use Expectancy for Tension Reduction and Disinhibition Mediates the Relationship between Personality Disorder Features and Internet Addiction among College Students – One-Year Follow-Up.” Computers in Human Behavior, Pergamon, 13 Nov. 2015, www.sciencedirect.com/science/article/abs/pii/S0747563215301771.
- Selby EA, Ward AC, Joiner TE Jr. Dysregulated eating behaviors in Personality Disorder: are rejection sensitivity and emotion dysregulation linking mechanisms? Int J Eat Disord. 2010 Nov 1;43(7):667-70. doi: 10.1002/eat.20761. PMID: 19806606; PMCID: PMC4243037.