Written by:

Medically Reviewed by:
Last Updated:
February 14th, 2025
OCD & Addiction
When people think of OCD, the image of someone who can’t stop cleaning often comes to mind. While this is true for some, there are many other aspects of OCD that go unnoticed. What’s less commonly known is the strong link between OCD and addiction, making this connection an important topic to explore. On this page, we’ll take a closer look at OCD and its relationship with addiction, uncovering how and why the two often intertwine.

What is OCD?
Obsessive-Compulsive Disorder (OCD) is a mental health condition where a person experiences recurring, unwanted thoughts (obsessions) and repetitive behaviours or rituals (compulsions). These obsessions and compulsions can take up a lot of time and cause significant distress, making it difficult for the person to go about their daily life.
People with OCD might have thoughts or fears that they can’t seem to shake, like worrying that something bad will happen if they don’t check the stove multiple times or feeling the need to wash their hands to avoid germs repeatedly. These compulsions are their way of trying to manage the distress caused by their obsessions, but over time, the rituals can become all-consuming.
Are there different types of OCD?
Because OCD is so personal, it’s possible for someone to develop obsessive thoughts and compulsive behaviours around almost anything. However, there are a few common areas that tend to be linked to OCD:
- Contamination fears: People may worry excessively about germs or cleanliness, leading to behaviours like repeated hand washing or cleaning. For example, someone might wash their hands until they’re raw after touching a doorknob, fearing they’ve come into contact with harmful bacteria.
- Checking rituals: This involves repeatedly checking things to prevent a perceived danger. A person might check their front door multiple times to make sure it’s locked, even if they know it already is.
- Symmetry or order: Some people feel the need for things to be arranged in a specific way and if anything is out of place, they feel intensely uncomfortable. For example, someone might constantly adjust picture frames until they’re “just right.”
- Unwanted thoughts: These can involve intrusive, often disturbing thoughts or fears that go against a person’s values, such as thoughts of harming someone. A person might avoid knives or sharp objects, even in harmless situations, due to these thoughts.
Everyone’s experience with OCD is unique, but by showing these examples, we aim to show how varied the condition can be.
Is having OCD dangerous?
Being diagnosed with OCD isn’t damaging in itself, but the actions a person with OCD may engage in can sometimes cause harm. For instance, someone with contamination OCD might wash their hands so frequently that their skin becomes cracked and painful. Or, someone with checking OCD might lose hours of sleep every night, constantly verifying that appliances are off or doors are locked, leaving them physically and emotionally exhausted.
Emotionally, the compulsions can also lead to feelings of shame, frustration and isolation, as individuals might feel embarrassed or misunderstood by their own behaviour. In some cases, this distress can become so overwhelming that people with OCD may turn to substances to quieten their intrusive thoughts and compulsions.
The link between OCD and addiction
Evidence from two large prospective cohorts clearly demonstrates a strong link between OCD and substance misuse. The study found that individuals with OCD are at significantly higher risk for developing alcohol and drug-related disorders.
Specifically, those with OCD were shown to have:
- A 4.5-fold increased risk of developing alcohol-related disorders
- A 6.7-fold increased risk of developing any drug-related disorder
- A 1.2-fold increased risk of substance use-related criminal convictions
- A 5.2-fold increased risk of substance use-related deaths
What’s particularly concerning is that these risks often manifest early, with the incidence of alcohol- and drug-related disorders becoming apparent as young as 16 years old.
This evidence highlights how obsessive-compulsive behaviours can drive individuals toward substance use as a form of self-medication, seeking relief from the relentless cycle of obsessive thoughts and compulsive actions. The higher risk of addiction and its consequences underscores the importance of addressing OCD early, with careful attention to the potential for co-occurring substance misuse.
Do I have OCD?
What may seem like a strange question to ask yourself is actually quite important. Many people go through life without ever realising that they have OCD, and research suggests it often goes undiagnosed. Recognising OCD early on can prevent potential social issues or even complications with addiction down the line.
To help, we’ve put together some questions. If you find yourself answering ‘yes’ to them, it might indicate a possibility of OCD. However, please keep in mind that these are not official diagnostic questions, and it’s important to seek advice from a medical professional for an accurate assessment.
Questions to consider:
- Do you frequently have repetitive, intrusive thoughts that you can’t control, even when they make you uncomfortable?
- Do you feel the need to repeat certain actions or behaviours to reduce anxiety, even when you know they don’t make sense?
- Do you spend a significant amount of time each day performing rituals or checking things (e.g., locks, switches, cleanliness)?
- Do you get distressed when things aren’t arranged in a certain way or don’t meet your standards of order or symmetry?
- Have these thoughts or behaviours started to interfere with your daily life, relationships or work?
If you find yourself relating to some of these questions, it’s worth speaking to a healthcare professional for a proper evaluation.
How can I get help for OCD and addiction?
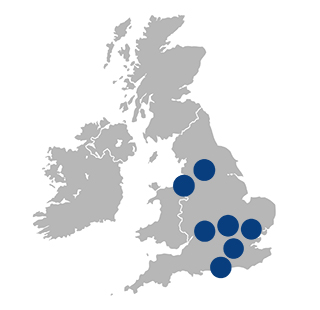
At Liberty House, both OCD and addiction are treated with a compassionate, dual-diagnosis approach, focusing on healing both conditions together for better results. The process often starts with a carefully managed detox (if needed), where medical professionals provide round-the-clock support to ensure comfort and safety.
Therapy is a vital part of recovery, where individual and group sessions help explore the root causes of both addiction and OCD. A key therapy used is Dialectical Behaviour Therapy (DBT), which helps you build the emotional skills you need to manage your OCD symptoms and addiction more effectively.
Holistic therapies, like yoga and meditation, are also woven into the programme to help reduce stress and promote emotional balance. These practices encourage self-awareness and resilience, helping you to cope with the challenges of both conditions.
Aftercare is the final step in the journey, offering continued group therapy and support. This creates a space where you can share your experiences and strengthen your coping strategies even after you finish the programme. Liberty House’s approach provides the care and understanding needed to help you manage both OCD and addiction for lasting recovery.
If you or someone you love is struggling with OCD and addiction, reach out to Liberty House today for further information on how we can help.
Frequently Asked Questions
(Click here to see works cited)
- Virtanen S, Kuja-Halkola R, Sidorchuk A, Fernández de la Cruz L, Rück C, Lundström S, Suvisaari J, Larsson H, Lichtenstein P, Mataix-Cols D, Latvala A. Association of Obsessive-Compulsive Disorder and Obsessive-Compulsive Symptoms With Substance Misuse in 2 Longitudinal Cohorts in Sweden. JAMA Netw Open. 2022 Jun 1;5(6):e2214779. doi: 10.1001/jamanetworkopen.2022.14779. PMID: 35666504; PMCID: PMC9171556.
- Brock H, Rizvi A, Hany M. Obsessive-Compulsive Disorder. [Updated 2024 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553162/