Written by:

Medically Reviewed by:
Last Updated:
February 14th, 2025
PTSD & Addiction
Living with trauma can feel overwhelming, and when it leads to addiction, the struggle becomes even harder to bear. Many people with PTSD turn to drugs or alcohol as a way to numb their pain, creating a dangerous cycle. Recognising this link is the first step toward finding the right support and getting help.
What is PTSD?
PTSD or Post-Traumatic Stress Disorder, is a mental health condition that can develop after someone goes through a deeply distressing or traumatic experience. This could involve anything from a serious accident or physical assault to combat or the sudden loss of a loved one. These events can leave lasting emotional scars and sometimes, the mind struggles to process what happened, causing PTSD to develop.
While PTSD can begin shortly after the event, it may also take months or even years for symptoms to appear. One of the most challenging aspects is that many people don’t immediately recognise that their current feelings are tied to past trauma.
Common symptoms include vivid flashbacks, unsettling nightmares and intense anxiety, often triggered by things that remind them of the event. People may also avoid certain places or situations, experience mood swings like irritability or depression or feel emotionally detached from others.
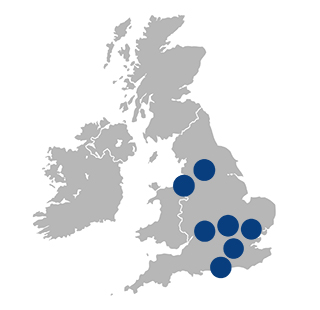
PTSD in the UK
PTSD affects far more people than many realise, and the numbers continue to rise. According to the NHS, around 33% of people who experience trauma may develop PTSD, though this figure can vary. One recent UK study, focusing on the aftermath of the COVID-19 pandemic, placed the prevalence of PTSD at 17.52%—double or even triple earlier estimates. This surge in numbers is a clear reminder that the impact of trauma can be more widespread and long-lasting than we expect.
In fact, an estimated 1 in 10 people in the UK will experience PTSD at some point in their lives, amounting to roughly 6.6 million people. Currently, PTSD affects around 2.6 million individuals in the UK, with many more being undiagnosed due to stigma or a lack of awareness around the topic.
Are there different types of PTSD?
PTSD is a complex issue, and simply saying someone has PTSD only scratches the surface. There are actually different subtypes of PTSD, each presenting unique symptoms and challenges.
Researchers have identified four main subtypes:
- Dysphoric (23.8%): Characterised by intrusive thoughts, avoidance, isolation and difficulty sleeping. Individuals in this group often experience depression, tend to be younger and are more likely to use nicotine.
- Threat (26.1%): Marked by high self-blame, negative emotions and hyperarousal but lower levels of isolation and irritability. This group often includes older individuals who have experienced natural disasters or injury to loved ones.
- High Symptom (33.7%): Exhibits elevated levels of nearly all symptoms and is more common among women and people with low income. Individuals in this group often report childhood trauma and have other psychiatric conditions, such as anxiety or depression. They frequently require therapy and medication.
- Low Symptom (16.3%): Features milder symptoms, with a focus on negative emotions and hypervigilance. People in this group often have higher incomes and better mental health, with fewer additional diagnoses.
Are PTSD and addiction linked?
Yes, PTSD and addiction are closely linked. Many individuals with PTSD often turn to substances like alcohol or drugs as a way to cope with the overwhelming distress and symptoms associated with their trauma.
This is known as the self-medication theory, which suggests that people with PTSD are at a higher risk of developing substance use disorders because they use these substances to try and manage their symptoms.
To further this theory, a study conducted at Grady Memorial Hospital in Atlanta, GA, recruited 587 participants from medical and OB/GYN clinic waiting rooms. When interviewed, it was found that:
- 39% were dependent on alcohol
- 34.1% were dependent on cocaine
- 6.2% were dependent on heroin/opiates
- 44.8% were dependent on marijuana
Studies have also shown that PTSD often appears before substance use disorders, further supporting the idea that people may use substances to alleviate their emotional pain. Unfortunately, this can lead to a cycle where substance use only worsens the underlying issues, creating an even greater struggle.
How is PTSD and addiction treated at Liberty House?
At Liberty House, we recognise that treating addiction alongside PTSD requires a specialised and compassionate approach. The complex relationship between these conditions means that individuals often face unique barriers during recovery, such as difficulties with trust, overwhelming emotions and recurring traumatic memories. Our PTSD and addiction programme is designed to address these challenges in a supportive environment.
Before starting treatment, it’s essential to consult with medical and mental health professionals to stabilise PTSD symptoms, allowing a better focus on addiction recovery. This may include therapy, medication or a combination of both.
Once symptoms are under control, we offer several therapies that not only help with addiction but also provide relief from PTSD:
Dialectical Behaviour Therapy (DBT):
DBT is particularly useful for individuals dealing with both PTSD and addiction because it helps them manage overwhelming emotions and impulsive behaviours, which are common in both conditions. The therapy focuses on teaching coping mechanisms, such as distress tolerance and emotional regulation, allowing individuals to better handle traumatic memories without turning to substances for relief.
Cognitive Behavioural Therapy (CBT):
CBT is effective for treating both PTSD and addiction as it helps individuals identify and challenge negative thought patterns that fuel both conditions. For those with PTSD, this may involve reframing how they perceive past traumas, while in addiction treatment, CBT can help change the thinking patterns that lead to cravings and relapse. The goal is to break the cycle of harmful thoughts and behaviours.
One-to-one counselling
One-to-one counselling offers a safe and confidential space for individuals to explore the unique ways their PTSD and addiction are interconnected. It allows them to work through trauma at their own pace, building trust with their therapist. This tailored approach ensures that both the underlying trauma and the addiction are addressed simultaneously.
Holistic therapies
Holistic therapies like art, yoga and meditation can be especially beneficial for individuals with PTSD and addiction. These therapies provide non-verbal outlets for processing trauma, which can be less intimidating than traditional talk therapies. Yoga, for example, helps reconnect the body and mind, reducing stress and anxiety, while art therapy allows individuals to express emotions they may struggle to put into words. These practices promote overall well-being, supporting both emotional and physical healing.
What’s next?
If you or a loved one is struggling with PTSD and addiction, don’t wait to seek help. At Liberty House, our specialised programme offers compassionate, integrated care to support both trauma and addiction recovery. Reach out today to start your journey towards healing in a safe and supportive environment.
Frequently Asked Questions
(Click here to see works cited)
- Schein, Jeffrey. “PTSD STATS.” PTSD UK |, www.ptsduk.org/ptsd-stats/. Accessed 14 Oct. 2024.
- “4 Possible Subtypes of PTSD.” Psychology Today, Sussex Publishers, www.psychologytoday.com/intl/blog/experimentations/202001/4-possible-subtypes-ptsd. Accessed 14 Oct. 2024.
- Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population. Depress Anxiety. 2010 Dec;27(12):1077-86. doi: 10.1002/da.20751. PMID: 21049532; PMCID: PMC3051362.
- Flanagan JC, Korte KJ, Killeen TK, Back SE. Concurrent Treatment of Substance Use and PTSD. Curr Psychiatry Rep. 2016 Aug;18(8):70. doi: 10.1007/s11920-016-0709-y. PMID: 27278509; PMCID: PMC4928573.